Aug 10, 2022
Do you suffer from persistent knee pain, especially in the front of your knee? You may be dealing with anterior knee pain, a common condition that can impact your daily life. Let’s dive into the potential causes and explore effective treatment options, including working with a knee pain physiotherapist for knee rehabilitation.
Causes of Anterior Knee Pain
Numerous factors have been linked to the development of anterior knee pain, also known as patellofemoral pain syndrome (PFPS). It’s important to note that while some have more concrete evidence than others, understanding these factors can help guide your treatment. Here are some key factors associated with anterior knee pain:
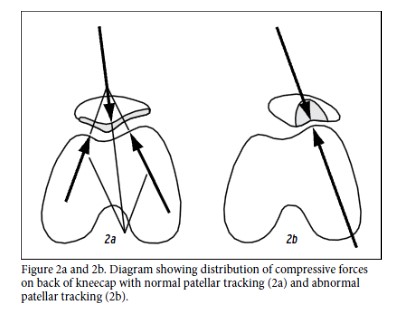
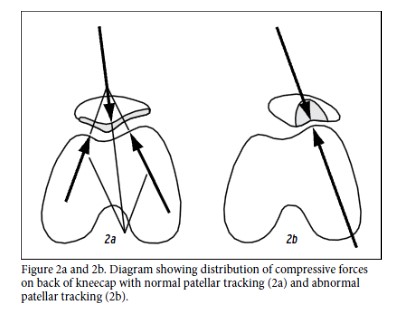
- Muscle Activation and Reflex Response: One important aspect is the activation and reflex response time of the vastus medialis (VM) in relation to the vastus lateralis (VL). Recent research has shown that individuals with PFPS may exhibit decreased electromyographic activity, small delays in muscle firing, or a combination of both. This can lead to abnormal patellar tracking and, subsequently, pain.
- Tightness in Muscles: Tightness in various leg muscles, including the gastrocnemius, hamstring, quadriceps, and iliotibial band, can also contribute to abnormal patellar tracking. These tight muscles can create biomechanical force vectors that result in lateral glide or other tracking issues, potentially causing knee pain.
- Quadriceps Strength: Weakness in the quadriceps, especially the vastus medialis compared to the vastus lateralis, has been identified as a potential factor in lateral patellar tracking.
- Hip Musculature Strength: Hip musculature plays a significant role in knee stability and patellar tracking. Weakness in the hip abductors and iliopsoas can lead to an anterior tilt of the pelvis and internal hip rotation, both of which can increase the Q angle and stress on the patellofemoral joint.
- Q Angle: A naturally large Q angle can lead to maltracking of the patella. This angle tends to be slightly higher in females, either due to differences in pelvis width or decreased height.
Effective Treatment for Knee Pain
If you’re dealing with anterior knee pain, it’s essential to explore effective treatment options. Working with a knee pain physiotherapist can be particularly beneficial. They can provide tailored knee rehabilitation strategies to address your specific condition. Here are some treatment approaches that can help:
- Muscle Strengthening: Our elite level Physiotherapists can guide you through exercises to strengthen the relevant muscles, such as the quadriceps, hip abductors, and iliopsoas, to improve knee stability.
- Sports Massage and Stretching: Targeted Sports Massage combined with stretching exercises for the gastrocnemius, hamstrings, quadriceps, and iliotibial band can alleviate tightness and reduce the potential for abnormal tracking.
- Patellar Taping: Taping techniques can be used to encourage proper patellar alignment during activities.
- Biomechanical Analysis: A knee pain physiotherapist can conduct a thorough biomechanical analysis to identify any contributing factors and develop a personalised treatment plan.
- Orthotic Support: In some cases, orthotic devices may be recommended to provide additional support and alleviate stress on the knee joint.
In conclusion, anterior knee pain can be a challenging condition, but with the right treatment, you can find relief and get back to enjoying an active lifestyle. If you’re experiencing knee pain, especially if it’s related to abnormal patellar tracking, consider consulting one of our expert knee pain physiotherapists at Physica Health in Bagshot for tailored knee rehabilitation and treatment for knee pain. Don’t let knee pain hold you back from the activities you love.
Book an appointment at Physica Health now to get on top of your knee pain. Call us on 01276916346 or Email info@physicahealth.co.uk
References:
Connelly et al 2009 Differences in patellofemoral contact mechanics associated with patellofemoral pain syndrome. Journal of Biomechanics. Volume 42, Issue 16, 2802-2807
Waryasz GR, McDermott AY 2008 Patellofemoral pain syndrome (PFPS): a systematic review of anatomy and potential risk factors. Dynamic Medicine.7:9:1-14

Aug 10, 2022
You may well have heard your Physiotherapist, Therapist or Doctor mention Inflammation when you have suffered an injury such as ankle sprain, knee ligament injury, back pain or even surgery but what is it? What is purpose of the inflammatory process and what does it mean for your injury? Read on to find out more…
An inflammatory response is usually initiated in a soft tissue when it is exposed to an excessive load that it is not usually used to (Solomonow 2009). In the case of a ligament, this can be a stretch type load when a joint is stressed beyond its limits.
The inflammatory response can be broken down into various stages which may slightly overlap. Watson (2003) describes 4 stages: bleeding, inflammation, proliferation, and remodelling. Initially whether it be a wound on the skin or damage to a ligament, this may well last for a few hours or more depending on the severity of the injury. This along with the subsequent stages all aim to clear away debris or dead cells and lay down new collagen and scar tissue to heal and repair the injured area (Watson 2003).
The inflammatory phase is one of the most important phases in tissue healing and is one that there has been much research into how it can be controlled and even inhibited with interventions such as prolotherapeutic and steroid injections respectively (Hauser & Dolan 2011). This stage includes an initial vasoconstriction of the blood vessels followed by a prolonged vasodilation for the rest of the inflammatory phase in order to increase the flow of the necessary chemical mediators, proteins, growth factors and mast cells to the injured area (Watson 2003). Polymorphonucleocytes (PMN’s) other phagocytic cells act to clean away debris and dead tissue while also releasing lactic acid which acts to stimulate proliferation and the next stage of the process (Watson 2003).
The proliferation phase then involves fibroblasts and endothelial cells moving into the damaged area, proliferating and laying down granulation tissue which will eventually form mature scar tissue. Blood flow is also gradually restored by the budding and growth of new capillaries from those already existing around the area (Watson 2003). The initial fibres are laid down in random orientation and are predominantly made of weaker type III collagen. Although this will eventually be remodelled into the stronger type one type collagen, the injured tissue or ligament will never regain its full strength (Frank et al 1999).
As its name suggests, the remodelling phase involves the remodelling of the scar tissue by improving its orientation in line with stress improving its strength and organisation. The overall strength of the ligament or tissue is also enhanced by the absorption of the type III collagen fibres that are then replaced by the more fit for purpose type I fibres. This phase has been reported to start within 1-2 weeks of the initial injury and can continue for a year or more depending on the severity of the injury and what further stresses are placed upon it (Watson 2003).
Overall, while the initial phases such as bleeding, inflammation and proliferation run their course in a matter of weeks, the process of remodelling can continue for up to 2 years as the body continuously turns over and tries to improve the collagen makeup and tensile strength of the affected tissue.
If you have any questions or would like help with your injury, then don’t hesitate to get in touch at info@physicahealth.co.uk or book a consultation with us online at www.physicahealth.co.uk
References:
Frank CB, Hart DA, Shrive NG 1999 Molecular biology and biomechanics of normal and healing ligaments – a review. Osteoarthritis and Cartilage 7: 130-140
Hauser RA & Dolan EE 2011 Ligament Injury and Healing: An Overview of Current Clinical Concepts. Journal of Prolotherapy 3(4): 836-846
Solomonow M 2009 Ligaments: a source of work-related musculoskeletal disorders. Journal of Bodywork and Movement Therapies 13: 136-154
Watson T 2003 Soft Tissue Healing. In Touch 104:2-9

Jan 7, 2021
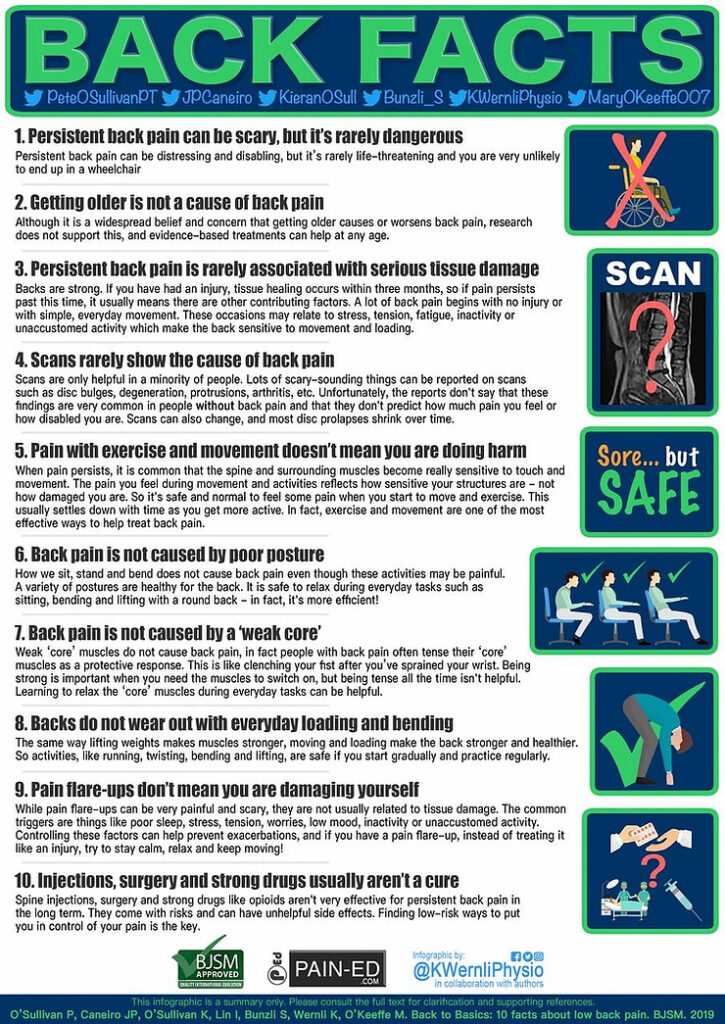
The world’s leading experts have compiled their top list of common misbeliefs and addressed them with some real world facts….
We can all take something from these…the over arching theme is that back pain is normal, it will get better and in general movement is good for us – its what we are designed to do!!
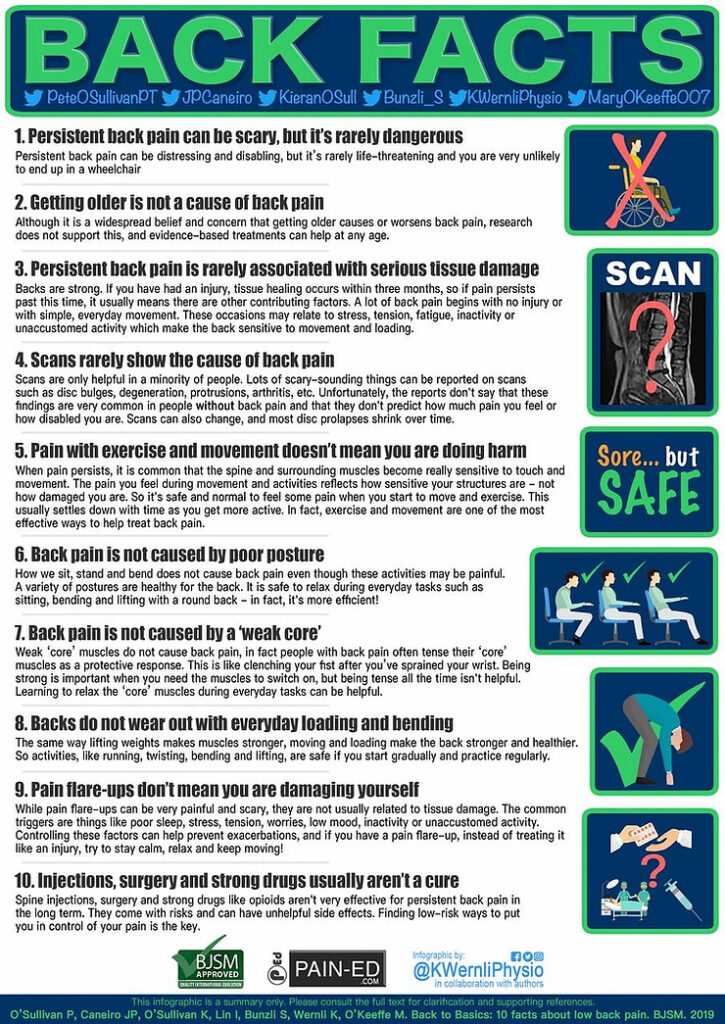
Back pain can be disabling, frustrating, stressful and impacts many aspects of people’s lives. Unfortunately almost 80% of us will experience back pain at some stage or another and it is the leading cause of disability worldwide. This can be driven by unhelpful beliefs in modern society that further compound the effects of this condition and impact recovery on individuals.
To combat this, some of the world’s leading practitioners (O’Sullivan et al 2019) have compiled some of the most common beliefs and responded with 10 facts about back pain. The more health professionals such as ourselves can incorporate these facts when treating our patients and clients the more we can gradually start to change people’s attitudes and improve outcomes.
We can all take something from these 10 facts – the over arching theme is that back pain is normal, it will get better and in general movement is good for us – its what we are designed to do!!
If you are experiencing back pain and would like to have a chat about these facts and how we can help, don’t hesitate to get in touch: info@physicahealth.co.uk 01276 916 346
O’Sullivan PB, Caneiro J, O’Sullivan K, et al Back to basics: 10 facts every person should know about back pain British Journal of Sports Medicine Published Online First: 31 December 2019. doi: 10.1136/bjsports-2019-101611
#lowbackpain #physio

Jan 7, 2021

Physica Health are delighted to announce a new initiative for this marathon training season. If a patient sees us as part of their preparation to run a marathon for charity we will to donate 10% of their total spend with us to their chosen organisation *.
We know first hand the work and training that goes into training for a marathon and understand there will be aches and pains along the way. Many runners need a little help from time to time… whether that be some physio, massage, advice or pilates and strengthening for running, we at Physica Health aim to be your one stop shop to help to get you to that marathon finish line.
Our experience in pro sport is second to none, helping us to advise you on your running preparation, planning and strength regime. Our Physio and director Vanesha has gone on the same journey by training for and completing her first London Marathon also. We feel this combination of expertise and experience together with an open door and availability to call in and chat about your preparation, excitement and any worries make us a great partner to have on your side for the journey.
If you need to spend money on physio or training to help you get through your journey then why not make sure some of it goes to your chosen charity.
Here is an overview of what we offer:
-
Physiotherapy – sporting and non sporting injuries
-
Pilates – We offer classes including Pilates for Runners. We also offer 1-1 sessions for Matwork and Reformer Pilates.
- Rehabilitation – We have extensive experience of rehab in pro sport as well as rehab studio with equipment on site.
-
Women’s Health – Therapeutic treatment of all disorders affecting the pelvis and pelvic floor, including pregnancy related problems.
-
Occupational Health – We can work with companies to provide wellness workshops as well as pilates and flexibility classes.
-
Athletic Screening – We use our pro-sport experience to screen for flexibility and strength imbalances that can be targeted to reduce injury risk.
-
Performance – Our strength and conditioning experience means we can put bespoke programmes together to assist with running performance and injury reduction.
We pride ourselves in offering:
-
A local ‘go to’ service that can offer treatment and advice with the same community feel as your running club or friends.
-
Quick service: we can usually get your clients seen within 48 hours.
-
We are covered by all major health insurers (*5% donated to your charity if using these)
Should you require any more info don’t hesitate to give us a call on 01276 916 346 or email us at info@physicahealth.co.uk
Feel free to take a sneak peak at our website www.physicahealth.co.uk
Wishing you the best of luck with your training
The Physica Health Team
#running #marathon #injury #physiotherapy #sportsphysio #charity

Jan 7, 2021
This article was featured on HADO’s website when they consulted with Damien on advice for low back pain….
To get some expert advice into the subject, we questioned Damien Kelly, Director and Physiotherapist at Physica Health in Bagshot, Surrey about how 10 different everyday tasks can exasperate existing back pain, giving tips for those suffering about how they might be able to minimise their discomfort during these activities. Back pain can be a debilitating condition, affecting your daily life and overall well-being. If you’re in Bagshot and suffering from back pain, it’s crucial to understand effective back pain treatment options and find the right back pain physio near you for expert guidance and back pain physiotherapy. Let’s explore how to manage your back pain and improve your quality of life.
- Sleeping and Back Pain
A common issue for many is the impact of sleeping positions on back pain. Achieving a restful night’s sleep is crucial, especially if you’re dealing with back pain. The ideal sleeping position for individuals with back pain can vary based on its type and location. However, there are some general guidelines you can follow.
If you find that sleeping on your back is most comfortable, consider placing one or two pillows underneath your knees. This helps maintain the natural curve of your lower back and can reduce discomfort associated with back pain. The same applies to side sleepers. In this case, use two pillows beneath your top knee or sleep with your knees bent and a pillow in between. Such strategies help reduce rotation in the lower back while sleeping, providing relief to the lower spine and surrounding muscles.
It’s essential to listen to your body. If you wake up feeling sore or uncomfortable, it’s an indication that your sleeping position might not be suitable for your back pain.
- Toilet Habits and Back Pain
Believe it or not, even going to the toilet can exacerbate back pain. The position you adopt during bowel movements can be uncomfortable. The ideal position for opening your bowels involves sitting with your feet on a stool and leaning forward onto your knees with your elbows.
However, if you’re experiencing back pain, comfortably maintaining this position can be challenging. Some individuals may experience difficulty in opening their bowels due to an increase in analgesia. In such cases, it’s important to increase the amount of fiber and water in your diet, or consult a pharmacist for a suitable laxative.
Back pain can lead to tightness in aligned muscles, making it challenging to relax your pelvic floor and bottom muscles to pass a stool. In extreme cases, people may experience a loss of bowel and bladder control alongside their back pain. In such situations, seeking prompt medical assistance is vital.
- Bathing and Showering for Back Pain Relief
Hot water, in general, can have a soothing and relaxing effect on muscles that are in spasm. However, it’s advisable to wait 24-48 hours after the onset of back pain before using heat therapy, as it can exacerbate the inflammatory response if applied too early after injury. After this timeframe, both showers and baths can offer relief.
For those with local muscle spasm and pain, taking a sitting position in a bath can be beneficial. Immersing yourself in warm water allows your muscles time to warm up and relax, reducing the discomfort of back pain. However, individuals with disc-related back pain may find such positions painful. In this case, showering is a better option, allowing you to direct the flow of water over the painful area.
- Getting Dressed with Back Pain
Individuals suffering from back pain often find that activities requiring bending forward, which creates flexion in the lower spine, can aggravate their condition. Activities like putting on socks and shoes or straightening up after bending can be problematic.
If you’re experiencing such issues, it’s advisable to take your time while getting dressed and choose comfortable, easy-to-wear footwear and clothing.
- Driving with Back Pain
Driving can be painful for those dealing with back pain, primarily due to the prolonged periods in a fixed position. To minimize discomfort, especially on long journeys, consider taking regular breaks to get out of the car and move around.
Cars with bucket seats can be particularly challenging for back pain sufferers. You can try raising your chair out of the bucket position by using a seat pad. Many modern cars come equipped with built-in lumbar support, which you should utilize to support your lower back. Maintain your hips at 90 degrees to the back and ensure the back support is upright, promoting a supported sitting position.
- Sitting at a Desk with Back Pain
For individuals who spend long hours sitting at a desk, it’s crucial to find ways to alleviate back pain. If possible, alternate between standing and sitting during work by using a standing or height-adjustable desk or moving to a countertop periodically.
If you have to sit for extended periods, ensure you have a good chair with adequate lumbar support to keep you upright and close to your desk. Position your screen monitor at an appropriate height, allowing you to look straight ahead, and keep your keyboard and mouse close to your body to avoid reaching forward for prolonged periods. Some people find sitting on a Swiss ball for short intervals beneficial as it encourages movement and activation of the local spinal stabilizers in the back.
- Housework and Back Pain
For individuals with low-level back pain, performing light housework and cooking should be manageable. However, it’s essential to avoid sustained flexion or bending forward for extended periods as it can worsen your symptoms. Keep moving around and change positions frequently to reduce strain. If your back pain symptoms are aggravated by standing for extended periods, it might be more comfortable to perform tasks like chopping and food preparation while seated.
Heavy housework can be problematic for individuals with back pain, especially those involving repeated bending and heavy lifting. In such cases, it’s advisable to minimize heavier tasks as much as possible.
If heavy housework is unavoidable, break down the tasks to reduce the load. For instance, instead of carrying an entire load of wet washing out to dry, place a chair by the washing machine and individually transfer items to a basket on the work surface. Carry 2-3 pieces of clothing at a time out to the washing line, reducing bending and lifting.
For back pain sufferers with chronic discomfort, investing in a lighter hand-held vacuum can make vacuuming more manageable.
- Lounging on the Sofa with Back Pain
Even lounging on the sofa for extended periods can lead to stiffness and discomfort, especially if you have back pain. To prevent this, it’s essential to get up and move regularly. Take short breaks to perform gentle mobility exercises for your back or simply walk around. When sitting, avoid slouching and aim for a relatively upright but not rigid posture. Supporting your back’s natural curve with a cushion or pillow can help. If you have access to a futon, use it to support your feet. As with all advice about low back pain, discover the setup that works best for you, but remember to get up and move frequently.
- Exercising with Back Pain
Exercising with back pain can be challenging, but it’s possible with the right approach. Understand the exercises that work best for you and those to avoid. Typically, exercises involving loaded flexion should be approached with caution. This includes weightlifting exercises like squats and deadlifts, which place significant loads on the lower vertebrae.
While these exercises are fantastic for building strength in the general population, they are not recommended for those experiencing back pain due to the strain they put on the lower back. With guidance from a qualified health professional, it may be possible to reintroduce variations of these exercises over time. However, in the interim, consider alternative leg exercises like the leg press or seated variations, which allow you to gain strength without overburdening your lower back.
General cardiovascular exercise can also be beneficial, but the type of exercise should be chosen based on whether your back pain tends to occur more in a flexed or extended position. For those comfortable with flexion, cycling and static biking are suitable options, while walking, jogging, and using cross-trainer machines can be beneficial for those more comfortable in an extended position. Some individuals find relief by getting into the water or swimming pool.
Before and after exercise, include gentle low back mobility exercises and, most importantly, listen to your body. Assess whether you feel comfortable during and after your workout or if you wake up the next day with increased pain and stiffness. This will guide you in determining if your back is ready to continue with a particular type of exercise or if you need to adjust your routine.
- Intimacy and Back Pain
Studies have shown that people with back pain often engage in less sexual activity than those without. This can be attributed to various factors such as a loss of interest in sex, fear avoidance, low self-esteem, and the presence of pain. To enjoy a fulfilling sexual experience, it’s essential to adapt sexual positions according to the type of back pain you’re experiencing.
If your back pain is disc-related or worsens with forward bending, positions that require holding forward-leaning postures may not be suitable for you. In this case, opt for a supported position like the missionary position. Placing a pillow under your hips and knees can provide additional support.
If your back pain is aggravated by arching backward (often associated with facet joint problems, arthritis, or spinal stenosis), you may find the side-by-side spooning position more comfortable.
If you experience additional pain during intercourse, it’s advisable to stop, try a different position, or attempt intercourse at a later time. Pillows can be used to adapt positions and make them more comfortable. Focus on moving with your hips and knees rather than overusing your back. Use pain relief when necessary and consult a healthcare professional for guidance. Most importantly, maintain open communication with your partner regarding any concerns or worries related to back pain and intimacy.
For more information or to request any advice on the above – Contact Physica Health – London Road, Bagshot, Surrey, GU19 5HD. info@physicahealth.co.uk. www. physicahealth.co.uk
You can find out more about our Physiotherapy team here